Paradigm shift in managing Abdominal Aortic Aneurysm (AAA)
Aneurysm of aorta is not uncommon. The incidence is on rising trend in the past 3 decades. The aging population contributes this.
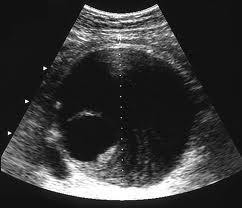
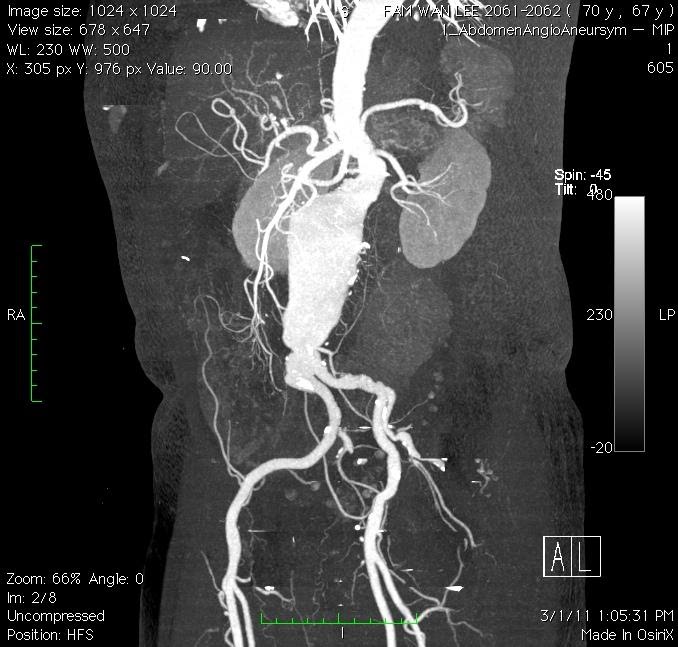
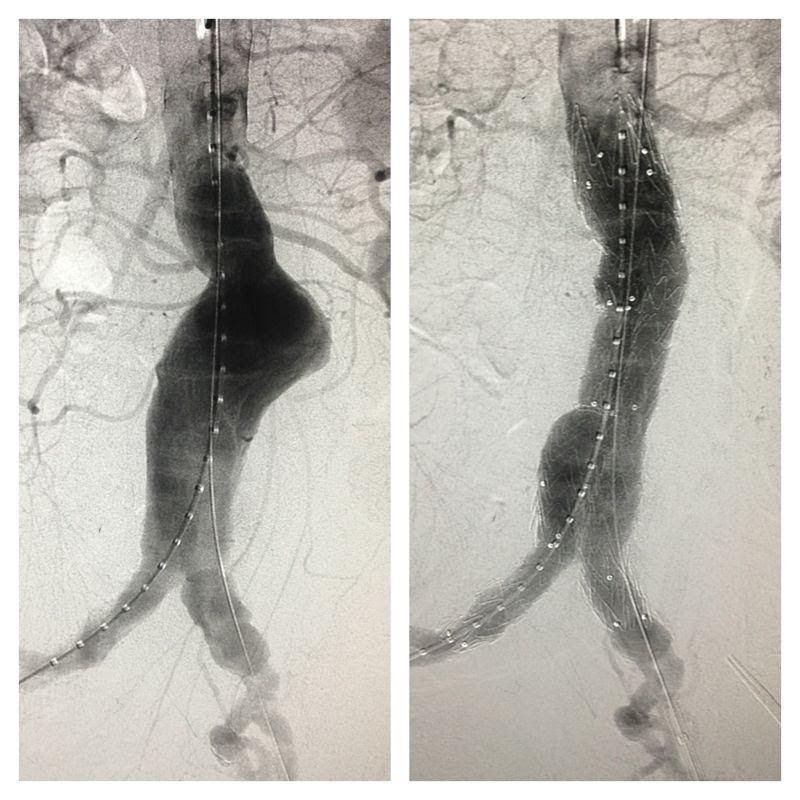
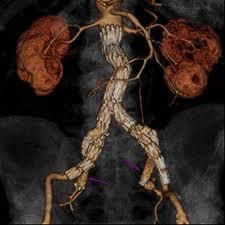
Modern diagnostic tools like ultrasonography (Figure 1) and computed tomography (CT) scan (Figure 2) makes the diagnosis much easier. The reported prevalence is around 4-8% in male and 1-2% in female after 70 year old. With ages beyond 80, the male to female ratio almost became 1:1.
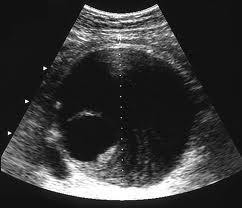
Figure 1. Ultrasonographic picture of AAA
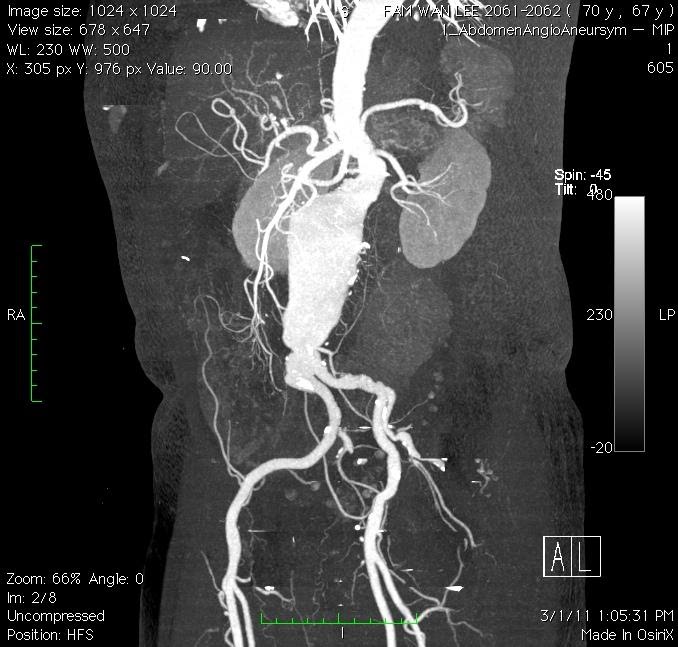
Figure 2. CT scan delineates the anatomy of AAA
When do we tell the patient his or her aorta is aneurismal?
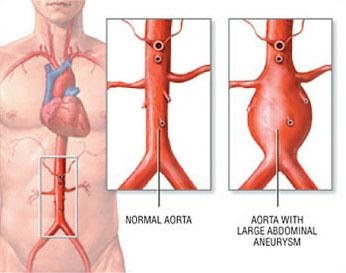
Abnormal dilatation of a vessel wall, more than 50% of its normal diameter is considered as aneurysm. Abdominal Aortic Aneurysm (AAA) is abnormal dilatation of abdominal aorta, more than 3cm in diameter. Commonest area involved is infra-renal aorta. (Figure 3)
Figure 3. Illustrating common site of Abdominal Aortic Aneurysm
Most of time Abdominal Aortic Aneurysm is picked up during routine abdominal scan for other reasons. Symptom of Abdominal Aortic Aneurysm is wide, from asymptomatic, upper abdominal discomfort, pulsatile abdominal mass (Figure 4), supra-umbilical abdominal pain, backache to peritonism.
It is lethal when the diagnosis is missed but not uncommon. Up to 25% of Abdominal Aortic Aneurysm cases are actually diagnosed when they start leaking.
Figure 4. Pulsatile abdominal mass
Traditionally, Abdominal Aortic Aneurysm cases will be observed from 3.0cm to 5.5cm, patients will be advised to continue on surveillance follow up and modifying their risk factors. Treatment will be planned when aneurysm size reaches 5.5cm.
Treating Abdominal Aortic Aneurysm has been challenging and multiple factors are taken into consideration before a diagnosis is confirmed. These include patient’s age, co-morbidy factors, symptoms and complications, the size of Abdominal Aortic Aneurysm and the morphology of the aortic sac.
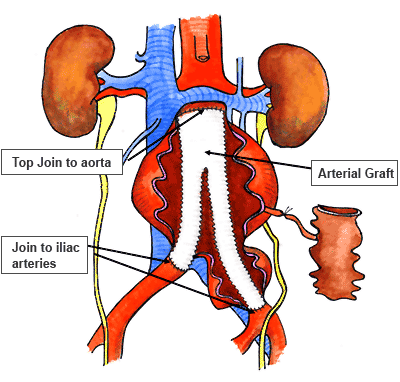
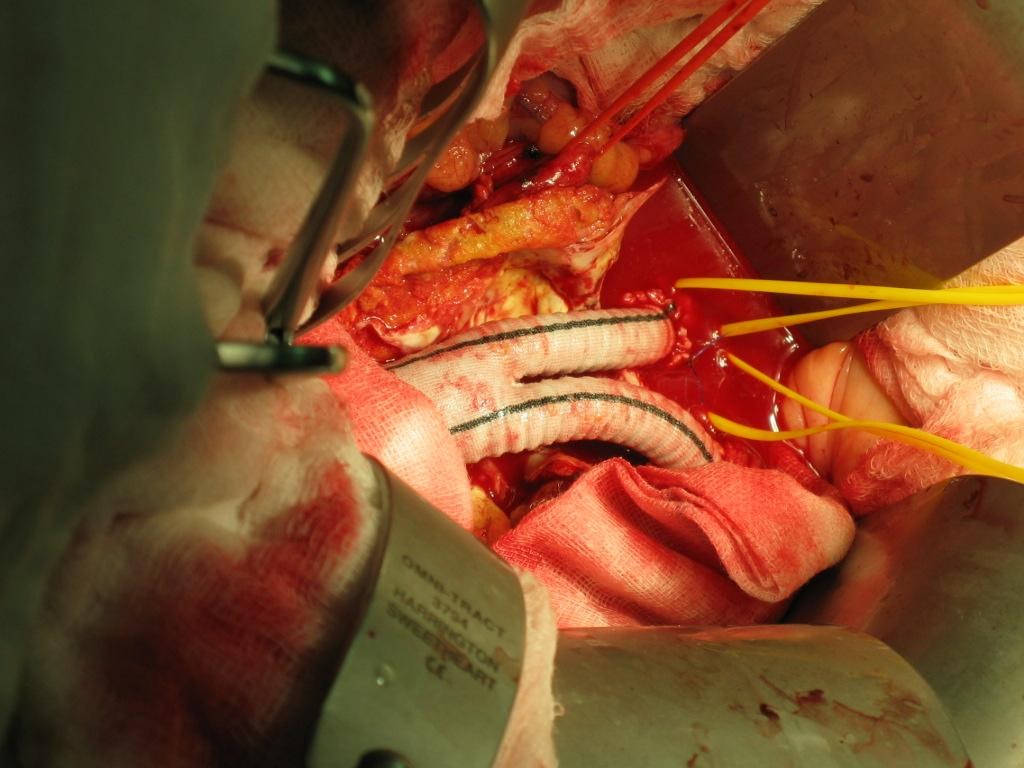
Ever since Juan Parodi put in the first stent graft in an Abdominal Aortic Aneurysm patient during 1990s, the status of open repair and inlay grafting (Figure 5,6) of Abdominal Aortic Aneurysm as gold standard has been challenged.
Endo-Vascular Aneurysm Repair (EVAR) has been popularized since 1995. Its outcome and durability has been proven beyond doubt in the past 20 years.
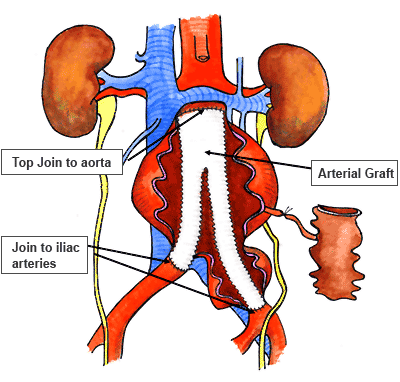
Figure 5: Cartoon illustrating open graft repair
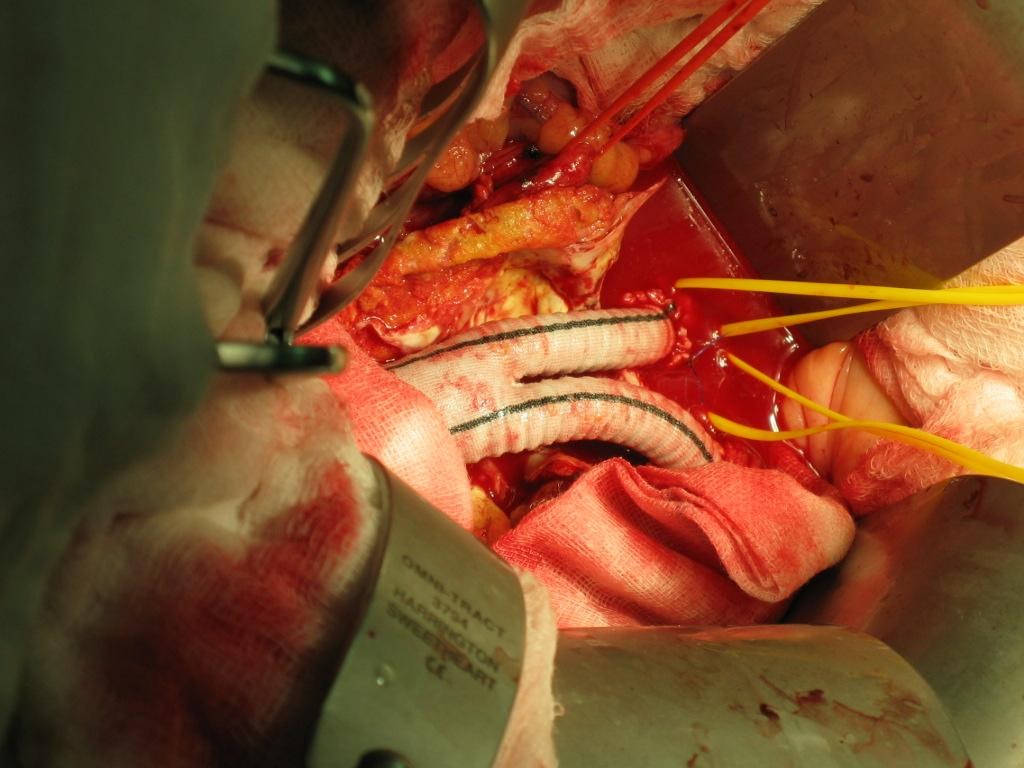
Figure 6: Intra-op picture of Inlay-graft
Open repair of Abdominal Aortic Aneurysm involves laparotomy, retroperitoneal access, cross clamping of aorta proximal and distal to aneurysm followed by aneurysectomy and inlay grafting. The peri-operative mortality started from 10% and surges with various co-morbid factors. It is not uncommon for a 70 years old AAA patient to present with Hypertension, Diabetes mellitus and Ischemic Heart Disease, as such the peri-operative mortality can be as high as 30-40%. The situation will be worst if patient first presented with leaking or contained ruptured AAA. Prolonged ICU stay post op with ventilator and dialysis support is needed in some cases.
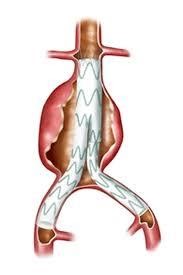
At the other hand EVAR procedure (Figure 7,8) involves access to femoral artery by cut down or percutaneous method, wiring into ascending aorta, tracking delivery device up into the aneurysm, stent graft deployment and then repairing the access femoral artery. The procedure avoided cross clamping of aorta and reduces blood loss intra-operatively. This help to maintain the hemodynamic during aneurysm repair, and hence reducing the stress to cardio-vascular system and to the patient as a whole.
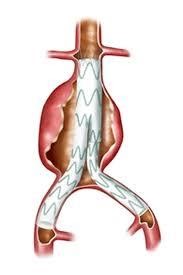
Figure 7: Cartoon picture of EVAR
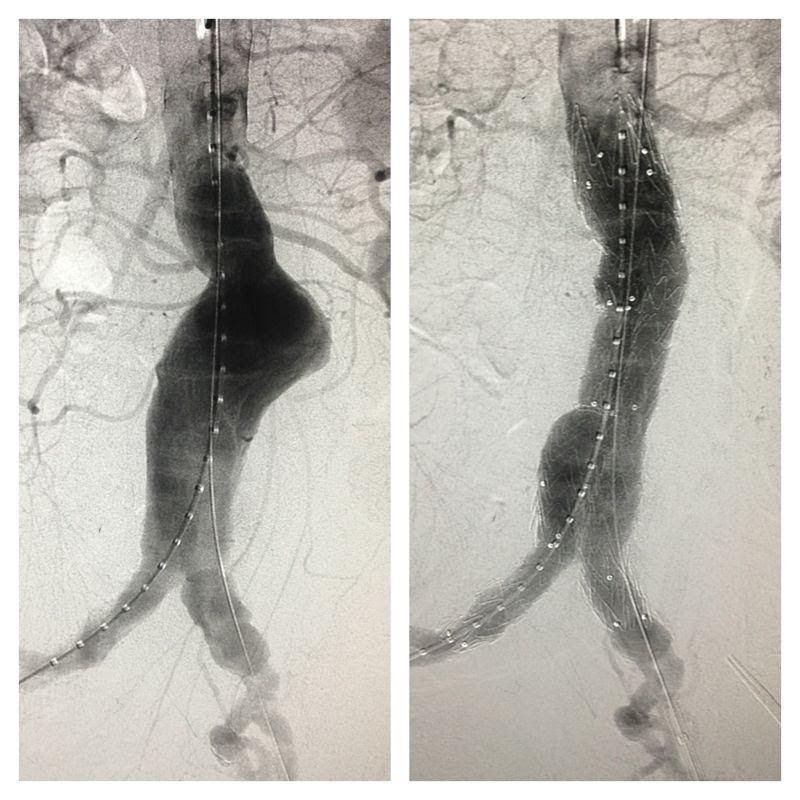
Figure 8: Angiographic picture of AAA, pre & post
As a minimally invasive therapy, EVAR greatly reduces the peri-operative mortality to around 2% and below. More importantly it reduces the ICU stay, reduces prolonged ventilation need, reduces blood transfusion and return the patient to normal life as soon as one can imagine. Its uses in ruptured or leaking AAA also improved patient’s survival rate and reduces the morbidity, even though the operative setting is different.
In order to prepare for EVAR, patient diagnosed with AAA needed a Computed tomography angiogram (CTA) with EVAR protocol. This enables the operative surgeon to calculate accurately on the size and type of stent graft needed, expecting possible difficulty and complication and hence improving the outcome of intervention.
The morphology of AAA is an important factor to decide on EVAR treatment. Infra-renal normal aortic segment of 20mm length, aneurysm-neck angle of less than 60 degrees, peri-aortic neck thrombus, tortousity of Iliac access artery and diameter of iliac artery used to be very strict criteria to decide on suitability of candidate for EVAR treatment.
However, with improvement of the device and stent design, further reduction in the delivery device profile, better interventional equipment and gadget, improvement in imaging quality, improvement in fluoroscopy facility and better operator’s skill and knowledge, the boundary is further pushed ahead. More and more patient with complex anatomy and marginal criteria can be accepted for EVAR treatment.
This indeed help a lot of previously declared not treatable AAA to be able to receive their treatment safely and effectively.
Aorto-iliac aneurysm treated with EVAR and bilateral Iliac bifurcation device and internal iliac stenting
Endovascular Aneurysm Sealing (EVAS) – another advance technology in solving aneurysm problem
Fenestrated EVAR (FEVAR) – providing solution for juxta-renal and supra-renal AAA
Our Doctor
Dr Syaiful Azzam bin Sopandi
Designation
Consultant General & Vascular Surgeon
Specialty
General Surgery,
Vascular Surgery