What to expect during your child examination
EYE examination for your child does not sound like an exciting activity one can do with their precious little ones, but it is as important as a regular check-up for further diagnosis, early detection or preventive measure. Depending on where you go for an eye check-up, it can be time consuming, tiring and frustrating for your little one.
As a paediatric ophthalmologist, we have seen many situations where a little patient throws tantrum or refuses to cooperate. Perhaps letting you know what an eye examination for your child entails might shape your expectation in terms of timing, complexity of the test or whether it will cause discomfort.
Book earlier time slot if possible. Children seems to be in a better mood when they are well rested and fed. First up, is a vision acuity test.
Vision Acuity Test
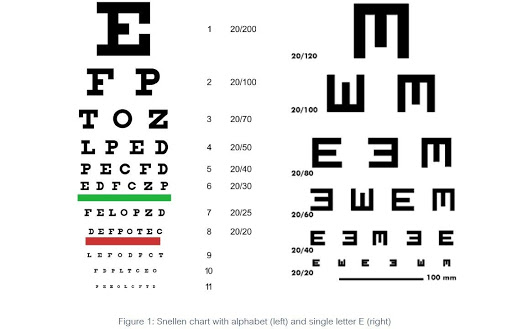
Snellen chart will help determine the clarity of your distance vision, suitable for any children over the age of 3. The child is required to stand or sit at 6m or 20ft away from the chart, which can be a wall-mounted chart or projected image at the wall. Those old enough to know the alphabets will read out the alphabet they see from top to bottom. The smallest row that can be read accurately indicates the visual acuity in that specific eye.
If you worry that the test might be affected due to the use of alphabet, the second chart with a single alphabet, such as the letter E can be used. The ophthalmologist can point Figure 1: Snellen chart with alphabet (left) and single letter E (right) to each letter on each line and ask the patient to point in the direction toward which the open end of the letter is facing.
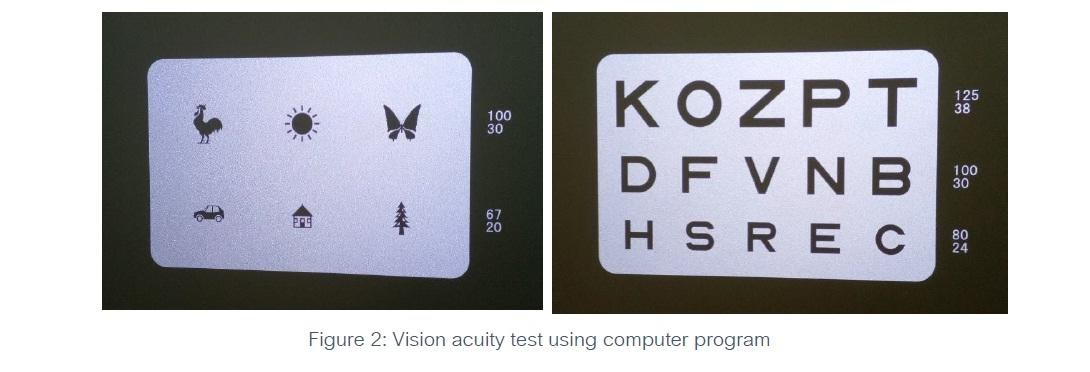
Next, similar vision acuity test using a computer, which can be programmed to have different type of test based on suitability of the patient. Smart kids will try to memorise the alphabet on the chart, so randomising them ensures no cheating in the test. Younger patients can be tested using pictures instead of alphabet, by recognising a simple picture at a certain size to indicate their vision acuity.
If your child does not seem to like reading alphabet aloud, fret not. There are many type of charts that are more exciting than an alphabet while being checked for their power. One such example is the Kay Picture Test below.
At the exam room, the child can sit on a chair or on the parent’s lap if preferred. The child will be asked to wear a special pair of glasses that have a space to insert lenses to check for their power, or diopters. Diopters or D is the unit used to measure the correction, or focusing power, of the lens your eye requires.
For much younger patients, if they can sit and able to hold their head upright, we can check their vision using Cardiff Acuity Test. It is a selection of preferential looking pictures designed to measure acuity in toddlers aged between 1-3 years or in individuals with intellectual impairment.
To test visual acuity of babies, that test combines the principles of preferential looking and vanishing optotypes, in which the value given is converted to Snellen equivalent. The test uses pictures that will interest a child (a house, car or duck for example) positioned either at the top or at the bottom of an otherwise grey card. There are eleven visual acuity levels, with three cards at each level.
For even younger babies, we can test their vision with toys, small object like raisins or a “hundred & thousand” sweet test. If the child is able to pick up a small sweet at 33cm, visual acuity is at least 6/24 or 20/80.
Refraction Test:
The second major test is a refraction test. Refraction is a process your eye-care professional uses to measure your refractive error or vision problem. For children 4 years and older or those able to co-operate, an autorefractor will be used to provide an objective measurement of a person’s refractive error and prescription for glasses or contact lenses.
During a comprehensive eye examination, the ophthalmologist will use refraction to determine how much power is needed to get your child perfectly focused vision. The comprehensive test consists of objective refraction and subjective refraction.
An objective refraction is a refraction obtained by using different instruments, such as retinoscope or auto-refractor, without receiving any feedback from the patient.
A subjective refraction requires responses from the patient. Your doctor may use a phoropter to measure your subjective refractive error.
A cycloplegic refraction is a procedure used to determine a person’s complete refractive error by temporarily paralysing the muscles that aid in focusing the eye. Sometimes eye doctors prefer to use this when trying to obtain an accurate refraction in young children who may skew refraction measurements by adjusting their eyes. To temporarily paralyse or relax the focusing muscle of the eyes, cycloplegic eye drops are used. To get the full cycloplegic effect or total paralysing of the eye muscle, more than a drop might be needed especially in heavily pigmented eyes, typical in Asian patients. we usually combine cycloplegic drops and dilating drops.
When a cycloplegic refraction is performed, the doctor can know what the full refractive error is without any influence of the person being tested. For example, the patient may be subconsciously over-focusing. This may make someone appear more near-sighted or less far-sighted than they are.
Cycloplegic eye drops do tend to sting for a few seconds when instilling them into the eye. Depending on the type of cycloplegic drop used, sometimes they have the temporary side effect of leaving the patient blurry for several hours. The patient could experience blurred vision even into the next day. Because cycloplegic eye drops also dilate the pupil, it will make the patient light sensitive for a few hours and protective sunglasses should be worn.
More Eye Examinations
Depending on age, the child might undergo a few more tests, such as slit lamp exam or bio-microscopy. The child will sit in front of an instrument with a space to rest his/her chin and forehead. A yellow dye called fluorescein, will be used to enhance any abnormalities on the surface of the cornea. Additional drops may also be applied to allow the pupils to dilate or get bigger. In this procedure, the child is required to look straight while the high intensity light is shined over the eyes. This basically gives us a closer look at the eyelids, conjunctiva, cornea, iris and lens. This dye drop, would not hurt as much, but the dilation drop might cause some sensitivity to light due to eye dilation which will pass over a few hours.
Once the eyes are dilated, I use this instrument on my head, called the indirect ophthalmoscope to examine the inside of the eye. It is valuable for diagnosis and treatment of retinal tears, holes, and detachments. The pupils must be fully dilated for it to work well. Setting up and getting the child ready and encouraging to cooperate takes some time, but getting a good view is important as well.